Young Athletes Part 3: Low Back Pain & Vertebral Stress Fractures (Pars Defects)
Words By Physio Samantha Yeung
 What if your Young Athlete has been coming home after training or sport complaining of ongoing lower back pain? At first they only mention it every now and then and you pass it off as “growing pains”. Then you realise, they are reporting it more following their sports participation, or possibly prolonged standing or walking (it may not just be complaining that they have to accompany you to do the shopping like you first think). Then it seems they are complaining more and the pain levels seem to be getting worse, and its now starting to affect their ability and train, and even their other daily life activities (hopefully they are not reporting pain at night waking them up – in this case we can assume the pathology is quite advanced which is a BIG problem!).
What if your Young Athlete has been coming home after training or sport complaining of ongoing lower back pain? At first they only mention it every now and then and you pass it off as “growing pains”. Then you realise, they are reporting it more following their sports participation, or possibly prolonged standing or walking (it may not just be complaining that they have to accompany you to do the shopping like you first think). Then it seems they are complaining more and the pain levels seem to be getting worse, and its now starting to affect their ability and train, and even their other daily life activities (hopefully they are not reporting pain at night waking them up – in this case we can assume the pathology is quite advanced which is a BIG problem!).
So you realise it has become significant and you finally go to Physio to get an assessment and diagnosis. What if that diagnosis is a “Pars Defect of the lumbar spine” (lower back)?
What is a “Pars Defect”?
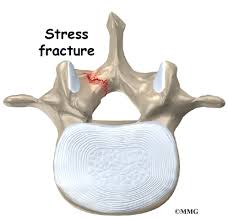 This is stress fracture of one of the vertebras of the lower spine – it can occur on one side, or both sides of the vertebrae. It is a relatively common cause of lower back pain in active and sporting children and adolescents that participates in sports – particularly those that involve repetitive backwards bending and rotating motions (think mostly Dance, Gymnastics, Cricket Bowling, Tennis, Volleyball and some Running Athletes).
This is stress fracture of one of the vertebras of the lower spine – it can occur on one side, or both sides of the vertebrae. It is a relatively common cause of lower back pain in active and sporting children and adolescents that participates in sports – particularly those that involve repetitive backwards bending and rotating motions (think mostly Dance, Gymnastics, Cricket Bowling, Tennis, Volleyball and some Running Athletes).
This repetitive movement pattern results in an overuse/repetition stress on the bony bridge of the vertebra called the Pars Interarticularis area. Hence it is referred to as a “Pars Bony Stress Injury” – which means the Bone is showing signs of stress, but not a discrete fracture line. Or if it is referred to as a “Pars Stress Fracture”, or a “Pars Defect”, this means on Imaging (MRI is best), there is the appearance of a discrete fracture line in the bone. This is not a good thing. And these injuries need to be taken seriously.
Why get an MRI?
An xray will not always show these injuries- and certainly won’t show the level of injury. An xray and CT scans also expose our Young Ones to radiation, so should not be the first Imaging of choice. An MRI will define the injury well, and shows us bones, muscles, & other soft tissue and does not expose our young athlete to radiation. Sometimes a CT scan localised to the area is ordered after an MRI if there is a need to further delineate if a fracture line is present.
What are the main symptoms?
As mentioned above, initially Coaches & Parents may commonly dismiss the symptoms as they may only be reported infrequently, and your Young Athlete might seem like they are still participating well in their sport. However, backwards bending activities (even looking up overhead) may bring on the pain.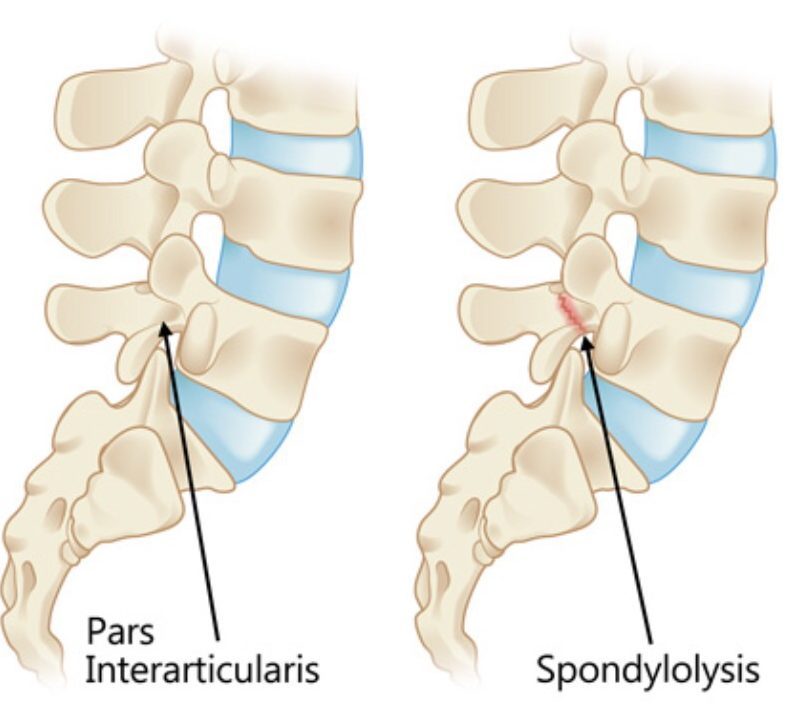
In all other activities and movements, only stiffness may be reported
Unfortunately, without an immediate appropriate management plan, pain can develop and progress quite quickly form the first onset of symptoms and may interfere with normal daily and school activities with large impact. When severe, your Young Athlete may have some level of constant pain that does not ease and wakes them at night. As a Physio, we know the recovery will be a long process when symptoms get to this level, so our biggest tip is:
take Low Back Pain in your Young Athlete seriously and get an early appointment with Physio and an accurate diagnosis and management plan put in place
How can physiotherapy help?
 Our Physio’s will help your Young Athlete by providing:
Our Physio’s will help your Young Athlete by providing:
- – An accurate diagnosis! You would be surprised how often GP’s, Coaches and Other Trainers miss recognising this injury, which is very unfortunate as an early diagnosis is usually associated with a faster rehabilitation period.
- – Collaboration with a Sports Physician (a Medical Doctor specialised in sports & exercise): our physios work alongside our sports physician to make sure your athlete gets the highest quality rehabilitation, which will include appropriate scans & further investigations, and may include bracing.
- – Education and advice on the necessary amount of rest and safe amount of exercises/ sports to gradually progress to.
- – Soft tissue therapy: to relief symptoms and tenderness around muscles, hips and upper back
- – Collaboration and communication with Remedial Massage Therapists: while our physios may initially perform soft tissue therapy to help relief acute symptoms , they may then communicate with our experienced massage therapist to facilitate deeper relief through the young athletes’ body as they return to levels of physical activity that may increase tissue tension
- – Rehabilitation: the mainstay of the conservative management can take anywhere between 3-6 months of a rehabilitation program, depending on the severity of the bone stress response. Rehab aims to build control and strength around the core/trunk of the young athletes, improve area’s where there may be reduced mobility, guide a safe return to activity and ultimately sport, and aim to prevent recurrence. Rehab will include a mixture of control-based movement exercises, then towards sports specific strength exercises and mobility exercises, and then into strength & conditioning.
If you are worried about your Young Athlete, and you need help from our experienced Physio Team or our consulting Sports Physician, phone us on 07 55006470 or Book for Physio online: www.mygcphysio.com.au
