GP Updates in Summary on Management of MSK Conditions

Guidelines for the Management of Low Back Pain
National Institute for Care & Excellence (NICE) recommendations for assessment & management of Low Back Pain & Sciatica in over 16’s – Read Here
Key Points
- Exclude specific causes of low back pain, for example, cancer, infection, trauma or inflammatory disease such as spondyloarthritis
- Consider using risk stratification (for example, the STarT Back risk assessment tool)
- Avoid routine imaging
- Consider Self Management, exercise programs, Manual Therapies – Consider manual therapy (spinal manipulation, mobilisation or soft tissue techniques such as massage) for managing low back pain with or without sciatica, but only as part of a treatment package including exercise, with or without psychological therapy.
- Promote and facilitate return to work or normal activities of daily living
- DO NOT offer Traction, Braces, Orthotics, Electrotherapies, Acupuncture
- Spinal injections – Do not offer spinal injections for managing low back pain.
- Consider Radiofrequency denervation, Epidurals under some circumstances
- See more regarding Surgical Intervention & Pharmacology Options

Shoulders
Rotator Cuff Shoulder Pain- to inject or not
J Orthop Sports Phys Ther 2019;49(5):289-293. doi:10.2519/jospt.2019.0607
Key Points
• As a result of a paucity of high-quality research in this area, it is not possible to make strong recommendations regarding the type, location, and technique of injection therapy in the management of Rotator Cuff Related Shoulder Pain (RCRSP).
• There is no clear consensus on the possible negative effects of corticosteroid injections on rotator cuff tissue.
• When compared to local anesthetic injections alone, corticosteroid injections may provide mild short-term pain relief for some patients with RCRSP. There is no evidence to suggest a difference between injection
types in the mid to long term.

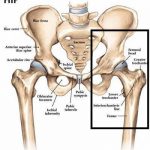
RACGP Guidelines for hip and knee OA management, Second Edition
Full Guide Here
Key Points Summary
Lifestyle:
• Regular exercise is important for relieving pain and improving function in people with knee and/or hip OA. For knee OA, land-based exercise such as muscle strengthening exercises, walking and Tai Chi are strongly recommended. Other land-based exercise that could be considered for some people with knee OA include stationary cycling and Hatha yoga. The best land-based exercise for people with hip OA could not be determined because of limited research. Aquatic exercise may be considered for some people with knee and/or hip OA.
• Weight management is strongly recommended for people with knee and/or hip OA who are overweight or obese.
Non-drug treatments:
• Cognitive behavioural therapy (CBT) could be considered for some people, particularly in conjunction with exercise, and taking into account existing mental health conditions, personal preference, cost and access.
• Heat packs or hot water bottles may be applied as a self-management strategy.
• Using a cane or other devices (eg walker, crutches) may be appropriate for some people with knee and/or hip OA to help improve pain, mobility and balance.
• A short course of manual therapy or massage could be considered for some people with knee and/or hip OA as an adjunct to lifestyle management.
• Transcutaneous electrical nerve stimulation (TENS) that can be used at home may be appropriate for some people with knee and/or hip OA.
• There is a conditional recommendation against the following treatments (refer to Section 3. Recommendations for an explanation on conditional recommendation)
– therapeutic ultrasound, – shockwave therapy, – laser therapy, – interferential therapy, – footwear marketed for knee OA, – cold therapy, – valgus braces and lateral wedge insoles for medial knee OA,
– patellofemoral braces, – kinesio taping.
Due to a lack of high-quality evidence, no recommendation can be made for the following
– formal self-management programs, – varus unloading braces and medial wedge insoles for lateral knee OA, – shock-absorbing insoles, – arch supports, – patellar taping, – pulsed electromagnetic/shortwave therapy.
Surgical interventions:
• There is a strong recommendation against surgery such as arthroscopic lavage and debridement, meniscectomy and cartilage repair for people with knee OA, unless the person also has signs and symptoms of a ‘locked knee’.
Read Summary Here

Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline
Full Guide Here
Key Points Summary that are New in this update:
-Participation in certain sports is associated with a heightened risk of sustaining a lateral ankle sprain.
-Care should be taken with non-steroidal anti-inflammatory drugs (NSAIDs) usage after an ankle
sprain. They may be used to reduce pain and swelling, but usage is not without complications and NSAIDs may suppress the natural healing process.
-Concerning treatment, supervised exercise-based programmes preferred over passive modalities as it stimulates the recovery of functional joint stability.
-Surgery should be reserved for cases that do not respond to thorough and comprehensive exercise-based treatment.
-For the prevention of recurrent lateral ankle sprains, ankle braces should be considered as an efficacious option.

Carpal Tunnel Syndrome: Clinical Practice Guidelines
Summary, Cochrane Review & Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health From the Academy of Hand and Upper Extremity Physical Therapy and the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2019;49(5):CPG1-CPG85. doi:10.2519/jospt.2019.0301
Here

BPPV Benign Paroxysmal Positional Vertigo: GP Summary
A Summary of Diagnosis, Assessment & Treatment of Benign Paroxysmal Positional Vertigo: HERE.
By Helen Sibbald– a Physio with special interest in Vestibular & Cervical Spine Management & Rehab
Link for the Consensus document of the Committee for the Classification of Vestibular Disorders of the Bárány Society -BPPV: Here